It is better to be healthy than ill or dead. That is the beginning and the end of the only real argument for preventive medicine. It is sufficient”1. This concise and clear statement of Geoffrey Rose, one of the pioneers of cardiovascular epidemiology and prevention in the last part of the 20th century may seem somewhat ironical during the Covid-19 pandemic, when an effective vaccination campaign2 is counteracted by a significant vaccine hesitancy3. But it underlines the need of an effective prevention in a setting which was defined the “perfect storm of rising chronic diseases and public health failures fuelling Covid-19 pandemic”3 by a Lancet press release illustrating the last reports of the Global Burden of Disease Study (GBD)4,5 updated to 2019. According to those GBD reports, leading causes of DALYs or health loss globally for both sexes combined, all ages, in 2019: were, after the first, neonatal disorders, driven by DALY definition, Ischaemic heart disease (2nd) and Stroke (3rd). Risks associated with the highest number of deaths worldwide, in 2019 were:
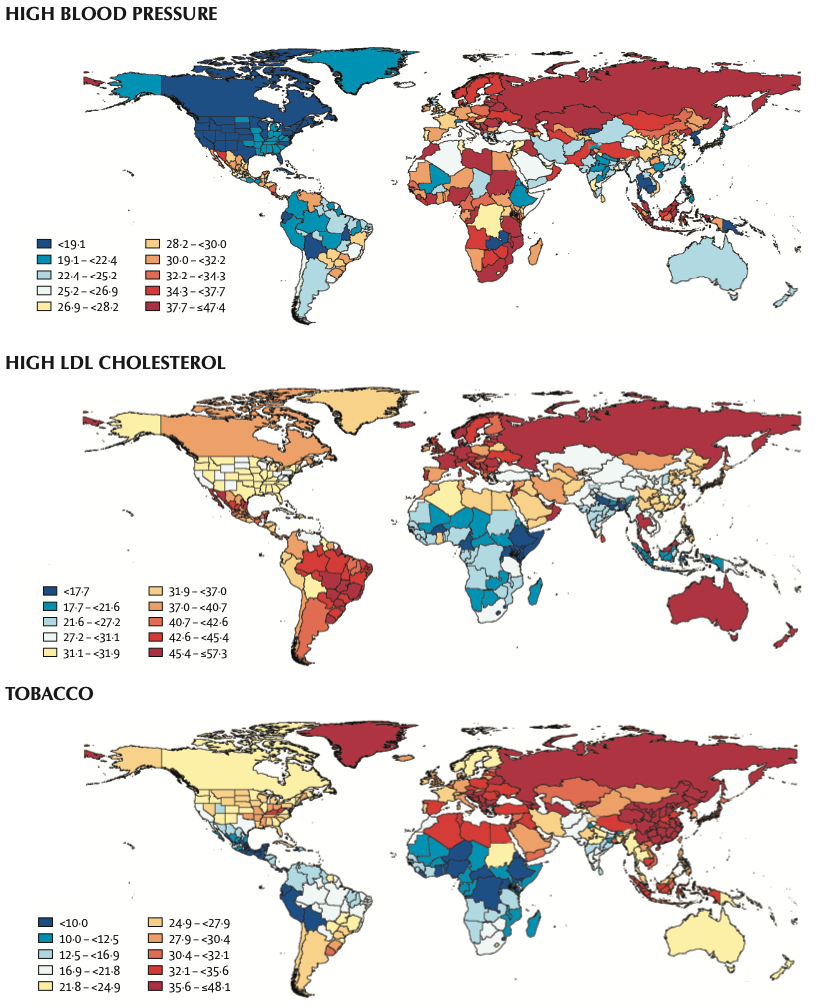
- High systolic blood pressure (10.8 million deaths);
- Tobacco (8.71 million deaths);
- Dietary risks (e.g., low fruit, high salt) (7.94 million deaths);
- Air pollution (6.67 million deaths);
- High fasting plasma glucose (6.50 million deaths);
- High body-mass index (5.02 million deaths);
- High LDL cholesterol (4.40 million deaths);
- Kidney dysfunction (3.16 million deaths);
- Child and maternal malnutrition (2.94 million deaths);
- Alcohol use (2.44 million deaths).
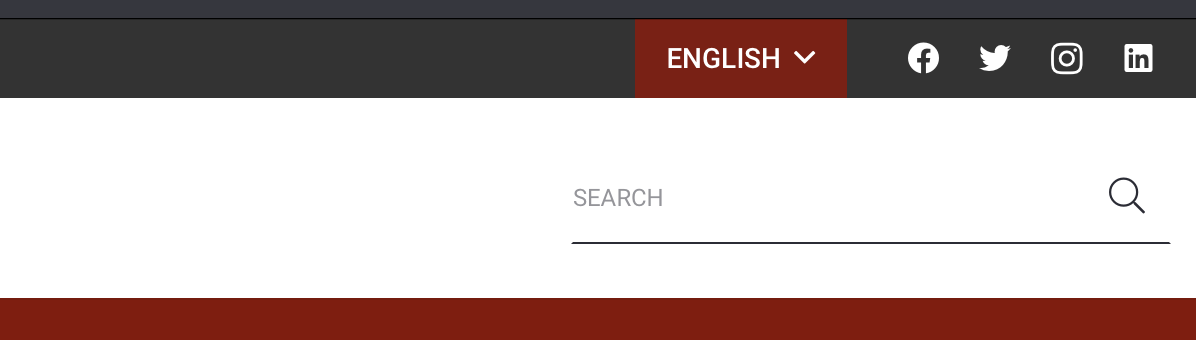
All those facts underline the need of an effective cardiovascular prevention all over the world, together with the efforts to curb the Covid-19 pandemic and to counteract the climate change. Certainly, prevention and surveillance policies should adapt to the different impacts of cardiovascular diseases and their risk factors in the various countries (Figure 1-2)5,6.
In this paper we will consider the results achieved and the possible future scenarios of cardiovascular prevention, which may be defined, adapting John Last’s words7, as a coordinated set of actions, at community and individual level, aimed at eradicating, eliminating or minimizing the impact of cardiovascular diseases (CVD) and their related disability.
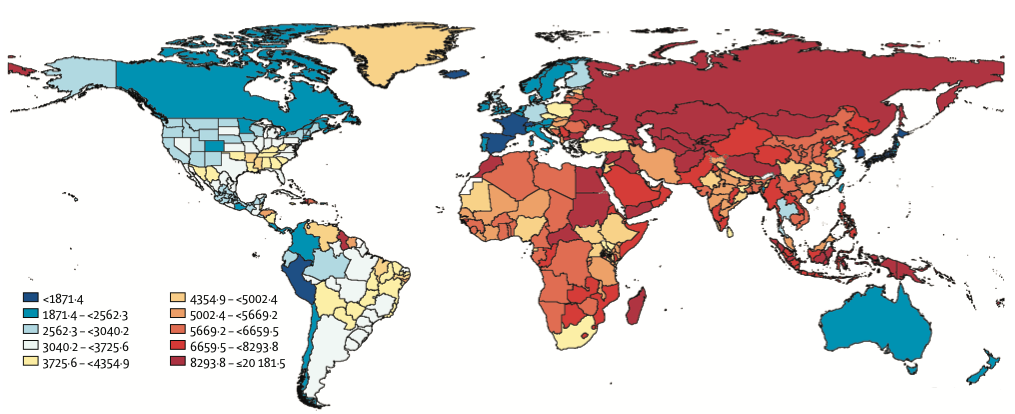
Fig. 1. Age-standardised DALY rates (per 100000) by location, both sexes combined, 2019 [derived from http://www.healthdata.org/results/gbd_summaries/2019/cardiovascular-diseases-level-2-cause].
SEV = summary exposure values, a measure of exposure to a risk factor normalized on a scale o 0 to 100 to make comparison possible between dichotomous, polytomous, and continuous risks by country or territory, and selected subnational locations.
Fig. 2. Age-standardised all-cause SEV by location, both sexes combined, 2019 [derived from http://www.healtdata.org/results/gbd_summaries/2019].
Results achieved by cardiovascular prevention
The bases of cardiovascular prevention are rooted in cardiovascular epidemiology and evidence-based medicine since 1961, when investigators in the Framingham Heart Study had shown that overtly healthy subjects with hypertension, hypercholesterolemia, and with smoking habit were at higher risk of developing an acute myocardial infarction8; they coined the term ‘coronary risk factors’9. There is evidence that lifestyles are responsible of levels of the risk factors10,11. In the following years many other concepts have evolved in CVD prevention, from the predictive value of coronary risk factors for other atherosclerotic diseases, like stroke and peripheral artery disease12 so they are termed “cardiovascular risk factors”, and from the notion of global CVD risk, to the Rose’s proposal1,13 of the two complementary approaches of “population strategy” (i.e. shifting adverse population risk distribution toward lower levels) and of “high risk” individual strategy, and to the Tom Strasser’s formulation of “primordial prevention” since pregnancy and childhood to prevent the development of risk factors14. More recently the attention was paid to the possible positive long-term consequences of favorable risk profile and to the issue of maintaining a low cardiovascular risk at all ages proposed by Jeremiah Stamler et al.15
Global CVD Risk Estimation and the low-risk approach
The global absolute CVD risk represents the likelihood of developing the disease over the following years, provided that the value of several risk factors is known. It is estimated through a risk equation using base-line risk factors and morbidity and mortality data of general population free of CVD at baseline and followed up in longitudinal studies. The risk equation includes: mean risk factors values of the population, risk coefficients, which attribute an etiological weight to single factors16, and survival probability. These elements change according to different populations, particularly when different cultures or generational cohorts are compared. The identification of CVD risk has become one of the main targets of primary prevention and the first step to reduce modifiable risk factors, from lifestyle changes to pharmacological treatments. Many tools were developed over time, including also the analysis of competing risks; the most recent ones are the SCORE217 and SCORE2-OP (older persons)18 in Europe, and the Pooled Cohort risk equations in the US, developed by a working group as part of the ACC/AHA 2013 Guideline on the Assessment of Cardiovascular Risk19 in the U.S. In Italy the Progetto CUORE20,21 allowed the development of a risk score and risk charts for men and women separately, considering the first major coronary or cerebrovascular event as the endpoint21 including age, systolic blood pressure, total cholesterol, HDL-cholesterol, smoking habit, diabetes, and hypertension treatment. The Progetto CUORE also allowed the researchers to evaluate the fate of the so-called favorable risk profile or “low risk” individuals22,23. This definition included persons with all the following characteristics: total cholesterol < 5.17 mmol/l (< 200 mg/dl), systolic blood pressure (SBP) ≤ 120mmHg, diastolic blood pressure (DBP) ≤ 80 mmHg, no antihypertensive medication, body mass index (BMI) < 25.0 kg/m2, no diabetes, no smoking; they were compared with individuals at “unfavorable but not highrisk” and at “high risk” – see the original articles22,23 for definitions. Low-risk individuals were only 3% at baseline, and they had virtually no coronary heart disease (CHD) and cerebrovascular diseases in the following ten years. The rates for unfavorable but not high-risk individuals (17% of the CUORE cohort) and high-risk individuals (80%) were higher and with a graded increase to one, two and three or more risk factors.
Epidemiological evidence of cardiovascular prevention effectiveness
While randomized double-blind clinical trials form the basis of treatment evidence in high-risk individuals, intervention programs at community level are much more difficult to perform and often with scarce results, as also recent experiences demonstrate 24,25, because of the influence of strong secular trends. Therefore it is better to rely on large standardized observational studies to evaluate prevention effectiveness. This is the case of the MONICA Study 26,29, more consistent than other modeling studies. According to MONICA data, regarding 36 populations in 21 countries of four continents, totaling 15 million people, in men CHD mortality rates decreased in 25 populations and increased in 11 populations; in women CHD mortality rates decreased in 22 populations and increased in 13 populations. In percentage terms, decrease in mortality rates in the MONICA data was less than that recorded in official mortality rates based on death certificate data. The MONICA Project demonstrated the substantial contribution of both decreased incidence and increased survival as well as the changes in the prevalence of risk factors to the declining trend of mortality: one-third of the decline in mortality was explained by changes in case fatality rates related to advancements in coronary care, two thirds by declining incidence in coronary events as partly explained by the reduction of classical risk factors.
In conclusion the lesson learned about CVD prevention demonstrates, in the continuum from primordial prevention to secondary prevention and rehabilitation, that primary CVD prevention driven by secular trends in lifestyle and clinical risk factors, played a major role in the CVD mortality decline in many populations, but its potential is much wider, aiming at reducing also the non-fatal CVD cases, other non-communicable diseases, premature and late disability, ensuring therefore a healthy aging to the majority of people.
Future directions in cardiovascular prevention
The results of the GBD study4,5 regarding 2019 indicate that there has been a substantial slowdown in the rate of decline of cardiovascular-disease (CVD) mortality in many high-income countries in recent years: this was most apparent at ages 35–74 years, where CVD mortality rates have increased in the USA (males and females) and Canada (females); high and increasing obesity, among other risk factors, jeopardize further CVD-mortality declines in many countries. Moreover the Covid-19 pandemic has a significant death toll worldwide29 and increases the burden of CVD30. Therefore there is a real need for innovative ways to create new approaches to CVD prevention, both in the realm of individual precision medicine and in the one of community intervention.
Precision CVD prevention from the polygenic scores to biomarkers, imaging techniques and artificial intelligence applications
A familial pattern in the risk of CHD was found in large studies involving twins and prospective cohorts 31,32. Since 2007, genome-wide association analyses have identified more than 50 independent loci associated with the risk of CHD33. These risk alleles, when aggregated into a polygenic risk score, are predictive of incident coronary events and provide a continuous and quantitative measure of genetic susceptibility33, which can identify subjects with a risk equivalent to individuals with familial hypercholesterolemia, but without an elevated LDL cholesterol34. A recent study confirmed that people with intermediate LDL levels (e.g. between 130 and 160 mg/dL), but with a high polygenic score, have the same risk as those with severe hypercholesterolemia35. The polygenic score can be used as an additional tool to support therapeutic decisions in people at intermediate risk, often difficult to reclassify with the other tools available36. Furthermore, statins and PCSK9 inhibitors were more effective in people with high polygenic scores, with higher benefits 37, 38.
Other research on coronary risk stratification or reclassification has focused, in addition to genetics and its scores, on biomarkers, in particular of inflammation39, on imaging both ultrasonographic 40, 41 and radiological42 and on their integration43, favored by computer applications defined “machine learning”44 an approach based on computer systems capable of learning and adapting without following explicit instructions, using algorithms and statistical models to analyze and drawing inferences from patterns in the data. Finally, “metabotypes” metabolic phenotypes are being studied to obtain “precision prevention”, especially from the food point of view45.
These scenarios are certainly interesting but two problems immediately emerge:
- once the best tools for “precision prevention” have been identified, their cost and their real applicability at the population level, in particular in primary prevention, must be assessed46;
- considering the population, the community context emerges also for the future, being an essential and non-reducible subject of prevention, as also the Covid-19 pandemic is demonstrating.
Community cardiovascular prevention in an epochal change
Individuals live in communities influencing their behavioral choices and here much remains to be done despite the evidence47 and the recent recommendations, both American48 and European 49,50. The issue is significant because even if genetic risk was evaluated in the Khera study33, among participants at high genetic risk, a favorable lifestyle was associated with a nearly 50% lower relative risk of coronary artery disease than was an unfavorable lifestyle. However, although there is evidence that lifestyle positive modifications can persist over time51, the majority of these intervention studies do not confirm this pattern if begun after childhood 24,25 hence there is a clear need for antenatal, perinatal and primordial prevention52. Another possibility to find new ways of intervention is to investigate in depth into positive “natural experiments”53 like the one occurred in Poland during the political transition54. Community cardiovascular prevention needs to be deeply innovated, integrating epidemiology, psychology, sociology, marketing science, statistics, informatics to find new ways to help communities to adopt a healthy lifestyle at every age, including pregnancy.